Blow fill seal technology is transforming sterile packaging with speed, safety, and repeatability that teams can trust today.
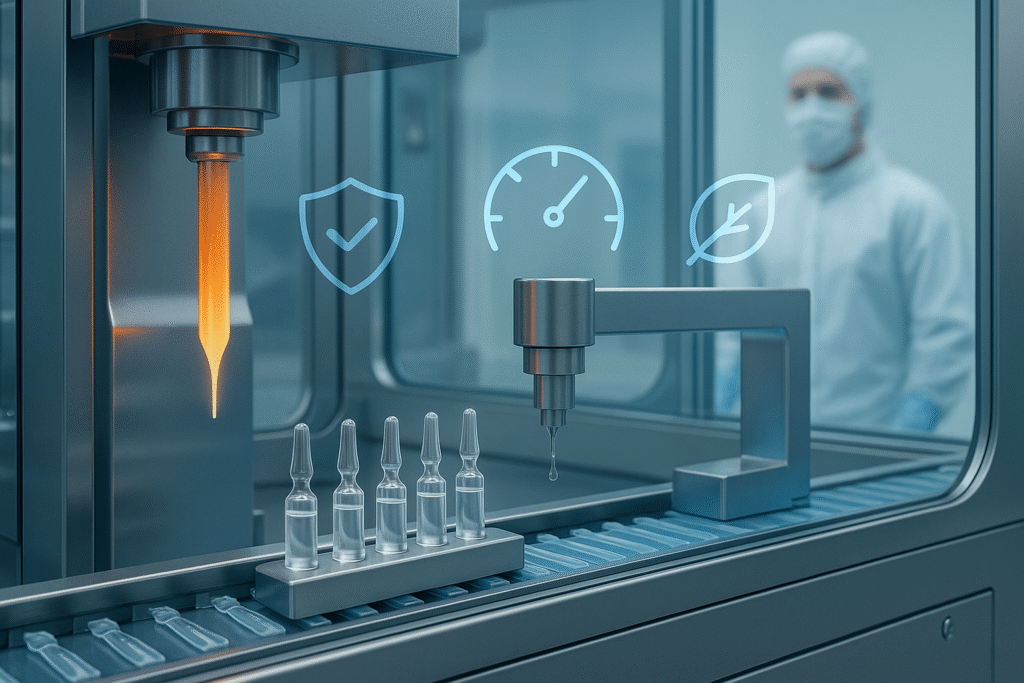
By forming, filling, and sealing in one enclosed cycle, BFS cuts contamination risks that slow launches.
Modern lines handle eye drops, inhalation solutions, vaccines, nutraceuticals, and sensitive diagnostics.
Operators benefit from minimal human intervention and automated CIP/SIP changeovers at scale.
Regulators appreciate the closed architecture and traceable electronic batch records in audits.
If you need sterile, scalable, and market-ready outputs, blow fill seal technology earns its place.
Why Blow Fill Seal Technology Wins
Why Blow Fill Seal Technology Wins?
First, BFS reduces human touchpoints, shrinking contamination pathways in a single integrated cycle.
Second, it compresses floorspace and utilities by replacing separate forming and filling suites.
Third, throughput climbs because micro-stops vanish when mold, fill and seal are synchronized.
Fourth, cost per unit drops as scrap, changeover time, and ancillary components all decrease.
Fifth, container design flexibility supports unit doses, twist-offs, ampoules and multi-chamber packs.
Sixth and seventh, digital sensors and PAT unlock predictive maintenance and continuous quality.
The Blow Fill Seal Technology Process Map
Following Are The Blow Fill Seal Technology Process Map:
Step one, plastic resin becomes a parison that enters a sterile mold under validated conditions.
Step two, sterile air shapes the container while controls stabilize wall thickness and geometry.
Step three, the product is aseptically dosed with mass-flow, time-pressure, or peristaltic systems.
Step four, the headspace is conditioned and the container is hermetically sealed in milliseconds.
Step five, in-line deflashing, coding, weigh checks, and vision systems verify each cavity.
Across all steps, blow fill seal technology uses closed loops that preserve sterility by design.
Blow Fill Seal Technology Market Signals To Watch
The Best Blow Fill Seal Technology Market Signals To Watch :
Large-volume BFS moves into biologics support fluids, diluents, and cold-chain ready formats.
CMOs expand BFS suites to serve mid-cap sponsors seeking faster technical transfers in 2025.
Sustainability rises with thinner walls, PCR blends, and energy-aware mold temperature profiles.
GEO-specific packs evolve for hot-humid lanes with barrier tweaks and UV-stabilized materials.
AEO and AIO schemas connect ERP, QMS, and LIMS to real-time release logic and dashboards.
Search interest for blow fill seal technology market and BFS solutions packaging keeps climbing.
4 Must-Know Rules: Compliance Frameworks That De-Risk BFS
Aseptic expectations align with ISO 13408-4, Annex 1, and cGMP interpretations on closures.
Risk management follows ICH Q9 and Q10 with robust change control and deviation trending.
Data integrity maps to ALCOA+ with secure audit trails inside validated MES environments.
Pharmaceutical critical process sealing is documented with leak, dye ingress, and CCIT evidence.
Materials, Molds And Container Geometry
Polypropylene dominates for heat tolerance while LDPE remains common for squeezable drops.
Multilayer barrier concepts add EVOH or tie layers where oxygen or aroma control is needed.
Neck finish and twist-off mechanics shape usability, opening torque and child resistance.
Mold cooling, gate design and venting influence clarity, flash rates and cycle economics.
Shelf-life modeling unites extractables, leachables and sorption with real-time stability data.
Human factors testing validates dose accuracy, grip comfort and tamper-evident signaling.
6 High-Impact KPIs: Validate, Monitor, And Improve BFS Outputs
Measure microbial recovery trends by intervention type to confirm state of control each run.
Track fill-weight Cpk, headspace O2 and seal strength to predict downstream stability.
Use vision defect Pareto charts to target flash, short shots and gate cosmetics by cavity.
Correlate line speed with reject rates to find the true economic sweet spot per SKU.
Quantify changeover minutes per format, then apply SMED to compress it quarter by quarter.
Tie complaints to root causes and CAPA cycles to close the loop in continuous improvement.
Conclusion:
Blow fill seal technology Wins blends sterility, speed, and design freedom that brands can scale.
If you manage ophthalmics, Blow Fill Seal Technology inhalation, or diagnostics, BFS reduces risk and improves UX.
A validated control strategy connects sensors, data, and release for reliable compliance.
Market momentum favors flexible, sustainable packs aligned to global GEO expectations.
Bookmark the resources below, then compare your current line to the 10-step roadmap.
Share this guide with teammates, leave your questions, and request a tailored checklist.
Table of Contents
What is blow fill seal technology?
Blow fill seal technology forms, fills, and seals a plastic container in one automated, enclosed cycle that limits human intervention and reduces contamination risk. The polymer is extruded into a tube, blown into a mold, filled with sterile product, then sealed—usually within seconds. This closed design is why regulators treat BFS as an advanced aseptic approach. You’ll see it most where sterility and speed matter. It also simplifies plants because one machine replaces multiple steps.
Where is BFS used most today?
Common uses include ophthalmic unit doses, respiratory and inhalation solutions, sterile saline and IV fluids; many firms also run nutraceutical and diagnostic liquids. B-F-S is attractive for unit-dose formats because containers are light and shatter-resistant. It scales from small ampoules to large-volume bottles without switching to glass. Adoption continues to rise as companies prioritize sterility and throughput.
Is BFS accepted by regulators for aseptic filling?
Yes. FDA guidance describes B-F-S as an automated aseptic process and applies the same sterile drug standards to it as other aseptic methods. In Europe, Annex 1 sets detailed expectations for B-F-S within sterile manufacturing, reinforcing contamination control and integrity testing. When you design your controls around these texts, inspections go smoother.
What materials do BFS containers use?
LDPE is common for squeezable, single-dose ophthalmic and respiratory packs; PP is selected when higher heat resistance or stiffness is needed. For better barrier, some designs add EVOH or similar layers to reduce oxygen ingress or aroma transfer. Material choice balances drug compatibility, permeability and user feel. Early extractables and leachables studies are essential.
Does BFS expose my product to damaging heat?
The mold must be hot enough to form the container but filling happens immediately after forming and can be engineered to keep product exposure brief. Suppliers tune parison temps, cooling and dwell times so liquids return to near room temperature quickly. For sensitive biologics, “cold” B_F_S variants and parameter optimization further limit thermal load. Always verify with stability and CQAs.
Can biologics and vaccines be run on BFS?
It’s feasible with the right controls. Industry case studies and CDMO experience show B_F_S handling of some biologics and vaccine presentations, provided heat, oxygen, and moisture are tightly managed. Pay attention to formulation, barrier needs, and real-time monitoring, then confirm via stability and integrity data. Not every molecule is a fit, so perform risk-based trials.
What does EU Annex 1 change for BFS operations?
Annex 1 emphasizes contamination control strategy across the line and adds a clear expectation for 100% integrity testing on containers closed by fusion, which includes B-F_S ampoules and bottles. Visual inspection alone is no longer enough for these closures. Plan deterministic integrity checks in-line or at release and document the method’s sensitivity.
Which CCIT methods work best for BFS containers?
Deterministic methods like high voltage leak detection and vacuum decay are widely used for liquid filled B-F-S. Helium mass-spectrometry offers ultra high sensitivity for special cases, while headspace analysis can support oxygen control. Current best practice favors deterministic, quantitative tests over legacy dye ingress whenever possible. Validate sensitivity to your product’s MALL.
How do you validate a BFS line for aseptic assurance?
Follow FDA aseptic guidance: qualify equipment, perform media fills that reflect real interventions, and prove your cleaning and sterilization steps. Map alarms and holds to a risk-based control strategy and show container-closure integrity per Annex 1. Keep robust environmental monitoring, then trend results to demonstrate a sustained state of control.
What clean and sterile utilities are typical around BFS?
CIP validates cleaning of product-contact surfaces, while SIP or equivalent sterilization readies the path before filling. In the sterile zone, firms often use steam or hot water on filling hardware and hydrogen peroxide for adjacent forming areas—within a controlled “tunnel” or enclosure. The goal is commercial sterility at startup and consistency during runs.
What container formats can BFS make?
From unit-dose twist-offs and ampoules to multi-dose bottles and infusion containers, BFS molds many shapes and volumes. The process is flexible enough to add features like droppers or connectors right in the mold. Container strength and shatter resistance help in shipping and cold chain. Choose geometry by dose accuracy and user handling tests.
How does BFS compare with traditional glass vial filling?
Because forming, filling and sealing are integrated BFS reduces manual touchpoints and related contamination paths. It can also boost uptime and cut floorspace versus separate forming and filling rooms. On the other hand, you must manage polymer permeability and potential thermal exposure. A fit-for-purpose risk assessment decides the winner per product.
What market trends are shaping BFS in 2025?
There is growing demand for ophthalmic and inhalation formats as well as lightweight, nonbreakable packs for logistics. Sustainability is driving lighter-weight compacting and optimized energy in molding. Annex 1st integrity trend is further driving the adoption of in-line CCIT, CDMOs are expanding their BFS capabilities to facilitate technology transfer and accelerate upgrades of BFS technology from development to production.
What are common pitfalls teams should plan for?
Watch for product polymer compatibility especially oxygen or moisture sensitivity that might be require barrier layers, control heat exposure during forming and verify no negative impact on potency for proteins and vaccines. Build deterministic CCIT early to avoid revalidation later. User testing should confirm opening torque and dose accuracy.
What is a simple roadmap to start with BFS?
Write a tight user requirements spec audit vendors for mold and CCIT expertise and prototype container geometry early. Align media fills with real interventions, validate CIP/SIP and connect MES or eBR for data integrity. Choose a deterministic leak test to meet Annex 1, Finish with stability, E&L and usability before PPQ.

